Blog
Tuesday, January 7, 2025
The Argument Against Extending ACA Subsidies
In what should come as no surprise, Republicans are warming to the expanded ACA that was designed, implemented, and already extended once by Biden along with the Democratic-controlled Congress. I recently wrote about how our elected officials have lost the ability to exhibit the responsibility and fiscal restraint that existed just a few decades ago, and this is yet another example.
These subsidies shouldn't be expanded for six reasons:
- The ACA was designed to increase subsidies as premiums rose and set definitions of affordability that ensured low-income Americans could afford to purchase insurance no matter the price.
- The ACA focused on people above the poverty line, and paid subsidies to people earning much more than the poverty level, even beyond the median household income.
- There is no reason that the affordability thresholds set by the ACA were too high and need to be reduced.
- Expanded subsidies have not led to uniform gains in coverage at all affected incomes, and the apparent gains are questionable.
- Increased subsidies will generally increase premiums, which will end up hurting taxpayers and people ineligible for subsidies while benefitting insurance companies.
- As always, given debt levels, spending more nonexistent money to make, at best, minor enhancements to a program with many other problems is unjustified.
ACA Already Set Subsidies to Make Health Care Affordable
One of the major features of the Affordable Care Act was the subsidies it paid to people earning too much to qualify for Medicaid, to be used to purchase insurance on the exchanges. The subsidies were designed on a sliding scale, to bridge the gap between what the ACA determined people could afford, and the current cost of insurance. The lower a person's income, the higher the subsidy. The higher their income, up to 4 times the federal poverty level, the lower the subsidy.
According to the original legislation, which Obama signed and every Democrat lauded for a decade, every American, regardless of their income level was expected to pay at least a little bit for their health insurance. For people making less than 133% of the Federal Poverty Level (FPL), Obama and Democrats believed contributing at most 2% of their monthly income was affordable. For a single-person right at the poverty line, that would amount to $20/month. For a family of four, less than $40/month. The government/taxpayers would pay the rest via a subsidy.
What often gets lost in discussions about ACA subsidies is that while these subsidies go to individuals and families who are low-income, they are not going to anyone living in poverty, by the government's definition. "% FPL" is a term used frequently in policy circles, but it's important to remember what it signifies--how much more income a person makes compared to someone living in poverty. The ACA, as originally legislated, focused its subsidies on Americans earning above the poverty level but no more than four times the poverty level.
In 2014, the median household income was $53,657 (2014 $), but subsidies were available to households up to 4 times the federal poverty level, which would amount to $71,040 for a household of 2.5 people (the national average). The diagram below shows how the subsidy availability compares to the income scale. In 2014, 300% FPL was pretty close to the median household income, meaning that subsidies were available well into the middle class of Americans.
One of the smart elements of the ACA was the definition of affordability was in terms of percentage of income. This produced several benefits. For one, it would prevent medical inflation from affecting the subsidy. For instance, if health care costs doubled, and premiums consequently doubled, while incomes remained stagnant, then the subsidy would cover the entirety of the premium inflation.
Defining affordability as the maximum percentage of income people should be expected to pay for health insurance meant that annual updates would be unnecessary and affordability would incorporate both the increase in health care premiums and changes in income. There would be little need to change it going forward. Beyond that, Democrats have been celebrating the slow growth of ACA premiums.
However, in 2021, for no particular reason, Biden and Democrats modified the thresholds so that, at every income level, the expected contribution of people to their health care premiums would fall, for most people by more than 50%, and for a large proportion, so that they were no longer expected to contribute anything. The expanded subsidies were only supposed to last through 2022, presumably covering the pandemic, but in the Inflation Reduction Act, the Democrats extended through 2025.
Affordability Redefined - Changes in Expected Contribution by Income Level

The table above shows the amount that people at various income levels were expected to contribute under the original ACA and under the expanded subsidies. President Obama and the Democrats of 2010 considered $25/month affordable for people just above the poverty threshold, and a gradually increasing amount for people making several multiples of that threshold. President Biden and the Democrats of 2021 substantially redefined affordability. In fact, Biden cut the expected contributions more if you were higher income than if you were lower income. While that may not be clear based on percentages, reducing contributions 4% for a higher income is a greater dollar reduction than for a lower income.
Also, bear in mind that these expected contributions are based on a Silver plan, which has higher premiums and lower out of pocket costs than a Bronze plan. Given Bronze plans are generally cheaper, in most cases, they would already be available for zero premium dollars for people between 100 and 200% of the federal poverty level.1
Like much of the other spending in the ARPA (for instance union bailouts, school slush funds, and an additional stimulus check), the expanded subsidies were not really necessary and were insufficiently debated and discussed, but got smuggled through because on their face, they seemed reasonable given the pandemic.
Subsidies Available to Way More Than Most Needy

Subsidies Raise Prices and are Captured by Corporations not Consumers
History has shown that subsidizing consumers often leads to increases in the list prices of the product. Sometimes, the increase in price completely offsets the subsidy meaning the money intended to help consumers ends up having no effect on their well-being at all, but goes to the company selling the product instead. This relationship has been borne out in education, housing, farm rental, child care, and solar panels.
Generally, this effect is more pronounced when supply of a good is limited, such as with housing or child care. In this case, while insurance products themselves are effectively unlimited, the premiums eventually go to a product that is limited - health care. To the extent that coverage leads to unnecessary utilization, it will lead to price increases for providers and premium increases for everyone.
Gains in Insured Population Are Questionable and Uneven
Since the enhanced subsidies, total ACA enrollment has nearly doubled, but looking more closely, gains have not been uniform across all the income levels. 60% of the growth in enrollment came from the 100-150% FPL and 71% of the growth came from people earning less than 200% of the FPL. On a per-beneficiary basis, these were the smallest changes in subsidy, but for these people their benchmark premium fell to zero. If the goal is to maximize enrollment, then dollars are best spent on the lowest income participants. This has the secondary benefit of being more in line with a system that focuses its social safety net on those most in need.
71% of the growth in enrollment came from the people who received the smallest boost in subsidies.
The Paragon Health Institute conducted its own review of the gains and compared to the number of people who would be eligible for subsidies at these income levels. They found that for many states, there was greater growth in enrollment than there were people in those states. They also found that reported incomes more often than would be expected, exactly matched the income thresholds that would warrant the subsidies. Consequently, they concluded that a 5 million of the newly insured were misstating their income to receive the subsidies. Before extending these subsidies, the government should redouble efforts to make sure only the people who deserve them are receiving them.
Further, there's reason to question the CMS enrollment numbers themselves. According to those numbers, ACA enrollment from people earning between 100 and 199 of the federal poverty level has more than doubled, adding millions of new beneficiaries in this group. The National Health Insurance Survey, though, shows no such growth in private ACA enrollment through 2023, the most recent available.
Insurance Coverage Levels for 0-64 year olds between 100-199% of FPL

Source: Lynn A. Blewett, Julia A. Rivera Drew, Miriam L. King, Kari C.W. Williams, Daniel Backman, Annie Chen, and Stephanie Richards. IPUMS Health Surveys: National Health Interview Survey, Version 7.4 [dataset]. Minneapolis, MN: IPUMS, 2024. https://doi.org/10.18128/D070.V7.4
The Ever-Present Debt
Lastly, of course, is the same argument against all new spending--there is no money to spend. Deficits are increasing more every year and will continue to for decades. New spending today will mean some combination of reduced services or higher taxes for the next generation. As with all spending, if you're in favor of this, if you think it is important and substantially beneficial, it should be no problem to name something that is less important, that is less beneficial, that is a worse use of money. Unless that can be named, and money shifted, then new spending should not be added.
Put slightly differently, and others don't report it this way, but every deficit dollar we spend today, is actually a commitment to spend more than double that over the next twenty years. It's a commitment to spend 7x that over the next 50 years, because every dollar we spend we have to borrow, and we never pay it back. So year after year, we're paying interest. Imagine you took out a 30k loan for a car that you didn't have to payoff for fifty years, and you never paid back the principle. You'd end up spending $213,000 over the fifty years and still owe more. The CBO predicts a baseline interest rate of 4% going forward, but there are many reasons to believe that that interest rate will increase as our debt increases and the United States falls deeper and deeper into debt.

As worrisome as the graph above looks, the reality will probably be worse because of the likelihood of higher interest rates as the debt mounts but also because CBO forecasts don't account for surges in spending due to recessions or spendthrift leadership.
Don't Extend the ACA Subsidies
There are plenty of reasons to be circumspect about the ACA subsidy expansion. Unfortunately, it's a lot easier to avoid careful review and not worry about the budget, the effectiveness of your spending, or fraud but bask in the adulation you get from blindly spending other people's money on a problem people wish was fixed.
Notes
1On average, Bronze plans' premiums are around $100 lower than Silver plans' premiums, so if your expected contribution is below $100 for the second-lowest cost silver plan, the subsidy you receive will be greater than the cost of the bronze plan.
Wednesday, September 25, 2024
The ACA Achieved None of Its Goals
It's been more than ten years since the ACA was fully implemented, and by most measures it has failed. In the 2008 election and the later part of 2009, healthcare reform was a top issue. For much of the campaign, before the financial crisis hit in mid to late 2008, it was the top issue. Candidates Obama and Clinton sparred frequently on the topic. The documentary film Sicko, Michael Moore's follow-up to his enormously popular Bowling for Columbine, and not quite as popular Fahrenheit 9/11 investigated the health care industry from many angles and served as a foundation for much of the criticism of the industry and urgency for reform.
The goals of healthcare reform were numerous. The overarching goal was to reduce the number of uninsured in the U.S. Almost as important was to reduce costs and improve outcomes. Few people have looked back at the full slate of goals of the ACA or the projections that accompanied it. Mostly, policy wonks focus on the one goal for which it was relatively effective and ignore the rest. Looking at all of the dimensions, though, and how they progressed over the past fifteen years shows that the ACA didn't solve almost any of the problems that were the biggest discussion points before the legislation even existed, and it often didn't meet the expectations set for it after it was written.
Uninsured
The primary goal of the ACA was to reduce the number of Americans who didn't have insurance. In the run-up to the legislative effort, the number of uninsured was ubiquitous in the news. While that goal was based on numbers that were greatly misrepresented (70% of the new Medicaid enrollees were eligible prior to ACA and chose not to sign up, and another large subset were illegal immigrants), even the expected reduction was never achieved.
CBO estimated that, by 2019, the number of uninsured would fall by 31 million. In reality, it fell by less than 15 million, before accounting for population growth and the booming 2019 economy. The Urban institute estimated a reduction of around 28 million.
Behind the numbers, Medicaid was expected to grow by 16 million, but it actually added 20 million more beneficiaries. The exchanges were projected to insure an additional 23 million Americans. By 2019, only 11 million people enrolled in an exchange plan.
The largest miss, and the biggest failure of the ACA is that it completely decimated the existing non-group insurance option. Before the ACA, there were approximately 15-17 million enrolled in private plans. By 2019, the combined enrollment in ACA and non-ACA plans was just under 19 million, meaning that the exchanges and subsidies did not generate much net improvement in the insurance rate because most of the ACA gains came out of or at the expense of the existing private plans.
Premiums
It's a universally acknowledged miss that President Obama promised that the ACA would "bend the cost curve down." He specifically said that the ACA would lower premiums for families by $2500/year on multiple occasions.
In 2017, Forbes published an article already calling into question this result.
Using National Health Expenditure Data provided by CMS, one can verify that the Forbes article was correct. Increases in private per enrollee costs grew faster after the implementation of the ACA. Costs for "Other Direct Purchase" which includes off-exchange plans, rose 5.4% per year from 2001 to 2013, and 8.6% per year from 2013 to 2022, after the ACA was implemented. Marketplace plans, specifically, have increased, on average 5.3% per year.

While the ACA was supposed to make insurance more affordable, the costs of insurance rose faster after its implementation compared to before. Everyone doesn't incur those costs equally, however. People who are insured through Marketplace plans may be eligible for some level of subsidy, depending on their income, which reduces the costs to them of the increased premiums. Those millions who are not eligible are now much worse off than they were before the ACA.

Costs for Exchange Plans are higher than the private, non-exchange plans
Note also that studies were done in 2013 projecting, due to experience up to then, that premiums would save even more money. Few studies have been done since, but every indication is that this was just a temporary phenomenon.
Outcomes
The most widely discussed health outcome prior to the ACA was US life expectancy. The fact that Cuba had a higher life expectancy than the US was frequently used to claim that the Cuban health care system was superior to the US's. Remarkably, since the passage and implementation of the ACA, life expectancy has improved at a much slower rate than before passage.

src: Data Commons
In addition to life expectancy, a primary goal of healthcare reform was to reorient care towards prevention and reduce emergency visits. According to CDC, the ED visit rate was unchanged between 2009 and 2019.
Conclusion
A careful review of the main healthcare challenges that were being discussed in the run-up to 2010, the problems politicians and media said would be solved shows that for every one of them, the ACA failed to solve the problem. In one case--the insurance rate--it helped, but in every other dimension--affordability, outcomes, appropriate coverage--it failed. Maintaining a rich skepticism of government's proposed solutions and their expectations cannot be emphasized enough.
Assorted Links
Obama's Broken Promises Blase - ACA and Trump RetrospectiveObama Healthcare Speech June 2009
Obama Healthcare Speech Sep 2009
Ben Bernanke Healthcare Speech 2008
Vance's statement about pre-existing conditions
New York Magazine - Vance wants to destroy healthcare
Side Comment on Using AI Resources
I'm not optimistic about ChatGPT or its competitors. There's clearly an existing internet bias towards the left, because the left produces more content. Try a google news search on a topic where you know there's a good right-leaning argument. You probably won't find it.
— Chris Oldman (@ChrisOldman4) September 27, 2024
As a side note, multiple AI chatbots said that the ACA did better at providing insurance, but wouldn't give me any source.
In addition, multiple said premiums have risen more slowly after ACA. One pointed me to this study done in 2013, before full implementation, and based on a weird metric, this study that reports individual year results, not the trend after ACA or before.
Tuesday, March 7, 2023
Did ACA Produce Free Healthcare?
An interesting observation was bouncing around Twitter over the weekend.
Fabulous point... in 2010 when Obamacare passed, health care was 17% of GDP and uninsured rate was 16%
— Timothy McBride (@mcbridetd) March 5, 2023
Today? health care 17% of GDP and uninsured rate is lowest ever: 8%!
See: https://t.co/athQpfpkww https://t.co/Q0SD1ObscA https://t.co/h8qMMiWVyg pic.twitter.com/CrEscJ8C4P
Left-leaning opiners are quick to attribute the success to the ACA, but it's not at all clear from the graph that this is what's happening.

Going back to 1990, the trend seems to be a sharp increase during recessions and then a gentle decline during expansions. This is true for 25 years up to 2015, when there's a slight bump up. Then, it begins another gentle decrease until the pandemic when it goes crazy. This graph certainly doesn't show that the ACA reduced health care costs.
But it's still an interesting observation that coverage is higher than it was despite the overall costs falling to pre-ACA levels. Despite the attempted attribution to the last major Democratic accomplishment, the cause is very difficult to pin down. The pandemic caused once-in-a-lifetime shocks to both healthcare and the economy. On the latter, there was a sharp decrease in GDP early-on, followed by an enormous stimulus that resulted in a quick economic recovery and then went on to cause a boom in demand that raised prices.
In healthcare, there was an immediate increase in demand for those who contracted Covid, but otherwise a sharp drop in healthcare demand as hospitals were not allowed to see non-Covid patients. Furthermore, policy changes in Medicaid and subsidies for the ACA upended the traditional coverage breakdown and also high employment would generally mean higher coverage through Americans' workplaces.
Two potential causes are services like telehealth, which is a lower-cost health care service, but this seems too small to account for a 2% of GDP drop in healthcare costs. A more likely cause is a shift from commercial to Medicaid. Medicaid reimbursements are infamously lower than commercial, so if more people switch from commercial insurance to Medicaid, high coverage rates would be achieved at lower cost.
The downside of this would be that providers would lose enormous sums of revenue. This can be tested by digging into the National Health Expenditures data.
The other potential cause is that healthcare coverage doesn't really mean anything. It's important to remember that having insurance does not necessarily equate to using healthcare services. Unless you have a chronic condition, visiting a doctor is a sporadic event. From 2001 to 2011 (for some reason the Obama Administration decided to stop producing these reports), the Census put out information on healthcare utilization. In 2011, the last available, 26% of people did not visit a medical provider at all; only 8% spent a night in the hospital; 57% did not take any prescription drugs.
Perhaps coverage increased, but it did not produce an increase in utilization. In fact, this theory is supported by the other graph in the Tweet.

Most of the drop in uninsured occurred in 2013. This marked the year both when subsidies kicked in for the healthcare exchanges and also when Medicaid expansion kicked in for the states that expanded.
But was there a simultaneous increase in healthcare costs? Looking back at the healthcare cost graph for 2013-2014, if anything, it shows a slight decline. This suggests that the explanation for the coverage/cost conundrum is that they are not strongly-linked. Particularly for Americans who are currently uninsured. It is a criminally under-reported fact that many who are not insured choose not to be despite having access to free or subsidized coverage.
Lastly, this entire observation may be ephemeral. The original graph of costs is not from CMS or a government agency, and thus is not the official value, but a non-profit organization's attempt to recreate it on a monthly basis. Their numbers are not quite the same as CMS for the years where they overlap, and notice that the graph goes into 2022, data unavailable through CMS. This wouldn't be the first time that pundits were quick to react to partial information that proved their point and then were proven wrong.
Thursday, March 2, 2023
Wasting Billions of Taxpayer Dollars - ACA Subsidies Edition
One of the reasons we have to go through a debt debate when we Republicans control Congress and Democrats control the Presidency, is because of how much money the government wastes in pursuit of its aims.
By waste, I do not mean only requirements piled on to subsidies, such as in the CHIPS Act, that diminish the effectiveness of the money funneled to them. I mean the government could spend less money and achieve the same result.
The Inflation Reduction Act's environmental provisions constituted a similar level of government waste in that the amount of money dedicated to reducing carbon emissions went beyond even the Biden EPA's astronomically high estimates of carbon emissions' costs.
According to several recent studies, Health and Human Services is getting in on the public funds bonfire by channeling large sums of money to insurance companies in the guise of "enhanced" subsidies to ACA Marketplace enrollees. If like most policy wonks, you measure the success of a policy by how many more people are insured, then the enhanced subsidies are an extravagantly bad avenue to pursue.
Two studies1 both found that poorly designed websites or portals imposed a hurdle for potential recipients significant enough to prevent many, particularly the young, poor, and healthy, from signing up for coverage. That automatically selecting a plan for would-be recipients is equivalent, in terms of increasing insurance coverage to lowering the premium by hundreds of dollars.
The American Rescue Plan Act and then the Inflation Reduction Act accomplished this feat by spending $25 billion per year (estimated) to subsidize coverage for people making up to more than $100,000/year. The same gains in coverage could be achieved much more cheaply through better program design.
Wednesday, February 8, 2023
Does Access to Medicaid Improve Health?
There have been several studies and politicians over the years purporting that health insurance, in general, and specifically Medicaid saves lives. A recent working study has found that, contrary to previous research, Medicaid expansions do not save lives. This result calls into question the numerous promises that were made in the ACA debate and foundations for a single-payer health system.
- Add Bernie Sanders claims about lives saved
- Medicaid promises during ACA debate
The canonical study on Medicaid was published in the New England Journal of Medicine in 2012. It found that Medicaid expansion led to a statistically significant reduction in "adjusted all cause" mortality. While the research was conducted after the passage of the Affordable Care Act, it was still before the implementation of Medicaid expansion, and consequently focused on pre-ACA expansions of Medicaid.
The small number of expansions is one of the primary reasons that the current study finds different results. The 2012 study was based on only three states, and furthermore, only found an effect in one of those states--New York. Drawing a conclusion for the entirety of the country based on the experience of only a single state, which is obviously not representative of the other 49 states in many ways, leaves ample space for over-interpretation of results.
Of course, the famous paper on the Oregon experiment in Medicaid expansion that found no effect is cited, yet appropriately caveated. The experiment wasn't large enough to detect small improvements and it was pretty soon after expansion, before there was enough time for improvement to occur.
Then there are two more recent studies on the ACA that found improvements in mortality of 3.6% for everyone and 9.4% for 55 to 64 year olds.
The authors of the new study focused on 8 of the 16 states that expanded Medicaid prior to implementation of the ACA. In true Brandeisian fashion, each state implemented its own version of Medicaid expansion--differing in the range of incomes affected, the years of implementation, the requirements, etc., offering researchers a panoply of variation from which to discern an effect.
They found that contrary to the other studies, those based on ACA and the one based on the three states only, that Medicaid did not reduce healthcare-amenable mortality, i.e. mortality that can be improved through better or more healthcare. This would include treating heart attacks or communicable diseases but exclude catastrophic car crashes and drownings, for example.
In fact, in none of the eight states that expanded Medicaid, was there an improvement in mortality that was determinatively produced by the expansion and wasn't just statistical chance. Reinforcing that result, without accounting for statistical variation, only three of the eight states even showed a reduction in mortality; the other five states had higher mortality rates after expansion.
To demonstrate that this study was an improvement on the previous three-state study, the authors even used their data and approach in an attempt to replicate the methods and results of its predecessor, and they succeeded. They found, just like the three-state study, that New York did show an improvement, and it was larger than the others. This provides support that the previous study was lacking in sample depth and rigor which led to a faulty conclusion.
Finally, the authors address the ACA studies and conclude that it is likely that the mortality effects are more significant for older populations but also that the other results may be partly driven by the non-expansion aspects of the ACA such as woodwork effects from the marketing campaign which would mean that mortality improvements could be achieved without expansion.
How Much has Zero Improvement Cost Us?
In 2013, the year of implementation of the ACA, approximately 18.7% of Americans were enrolled in Medicaid. In 2020, before Covid and its resultant legislation caused an increase in enrollment, that figure was 22.4%. So a cursory estimate is that the ACA led an additional 3.7% of Americans to enroll in Medicaid.
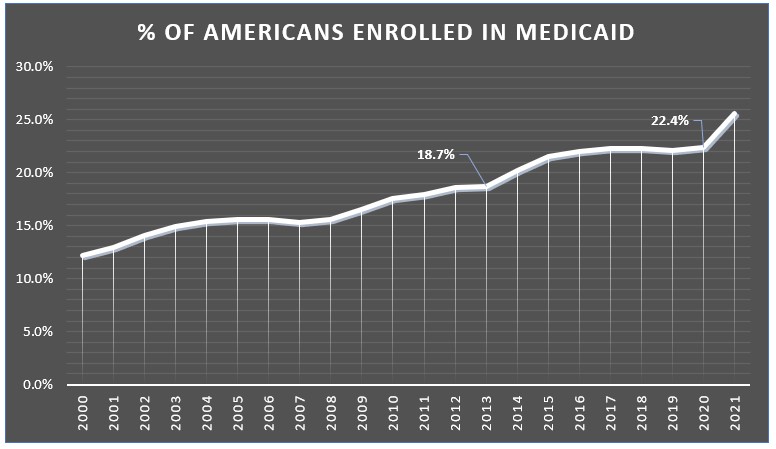
Multiplying that by costs per enrollee and the total population, the cost in 2020 for expanding Medicaid was $112 billion. Applying that same approach to every year from 2014 to 2021, a combined $700 billion has been spent without achieving any mortality benefits.
From 2014 to 2021, a combined $700 billion has been spent without achieving any mortality benefits.
Even if we assume a 10% improvement in mortality, higher than either of the studies that found an effect, this works out to saving 560 lives per year and spending $200 million per life saved1, 20 times the value used by the EPA in their recently proposed social cost of carbon update.
Had a 10% improvement in mortality been achieved, Medicaid expansion would have spent $200 million per life saved, substantially more than policy-makers deemed effective.