Wednesday, February 8, 2023
Topic: Policy
Content Type: Analysis
Keywords:
healthcare, ACA, Medicaid
Does Access to Medicaid Improve Health?
There have been several studies and politicians over the years purporting that health insurance, in general, and specifically Medicaid saves lives. A recent working study has found that, contrary to previous research, Medicaid expansions do not save lives. This result calls into question the numerous promises that were made in the ACA debate and foundations for a single-payer health system.
- Add Bernie Sanders claims about lives saved
- Medicaid promises during ACA debate
The canonical study on Medicaid was published in the New England Journal of Medicine in 2012. It found that Medicaid expansion led to a statistically significant reduction in "adjusted all cause" mortality. While the research was conducted after the passage of the Affordable Care Act, it was still before the implementation of Medicaid expansion, and consequently focused on pre-ACA expansions of Medicaid.
The small number of expansions is one of the primary reasons that the current study finds different results. The 2012 study was based on only three states, and furthermore, only found an effect in one of those states--New York. Drawing a conclusion for the entirety of the country based on the experience of only a single state, which is obviously not representative of the other 49 states in many ways, leaves ample space for over-interpretation of results.
Of course, the famous paper on the Oregon experiment in Medicaid expansion that found no effect is cited, yet appropriately caveated. The experiment wasn't large enough to detect small improvements and it was pretty soon after expansion, before there was enough time for improvement to occur.
Then there are two more recent studies on the ACA that found improvements in mortality of 3.6% for everyone and 9.4% for 55 to 64 year olds.
The authors of the new study focused on 8 of the 16 states that expanded Medicaid prior to implementation of the ACA. In true Brandeisian fashion, each state implemented its own version of Medicaid expansion--differing in the range of incomes affected, the years of implementation, the requirements, etc., offering researchers a panoply of variation from which to discern an effect.
They found that contrary to the other studies, those based on ACA and the one based on the three states only, that Medicaid did not reduce healthcare-amenable mortality, i.e. mortality that can be improved through better or more healthcare. This would include treating heart attacks or communicable diseases but exclude catastrophic car crashes and drownings, for example.
In fact, in none of the eight states that expanded Medicaid, was there an improvement in mortality that was determinatively produced by the expansion and wasn't just statistical chance. Reinforcing that result, without accounting for statistical variation, only three of the eight states even showed a reduction in mortality; the other five states had higher mortality rates after expansion.
To demonstrate that this study was an improvement on the previous three-state study, the authors even used their data and approach in an attempt to replicate the methods and results of its predecessor, and they succeeded. They found, just like the three-state study, that New York did show an improvement, and it was larger than the others. This provides support that the previous study was lacking in sample depth and rigor which led to a faulty conclusion.
Finally, the authors address the ACA studies and conclude that it is likely that the mortality effects are more significant for older populations but also that the other results may be partly driven by the non-expansion aspects of the ACA such as woodwork effects from the marketing campaign which would mean that mortality improvements could be achieved without expansion.
How Much has Zero Improvement Cost Us?
In 2013, the year of implementation of the ACA, approximately 18.7% of Americans were enrolled in Medicaid. In 2020, before Covid and its resultant legislation caused an increase in enrollment, that figure was 22.4%. So a cursory estimate is that the ACA led an additional 3.7% of Americans to enroll in Medicaid.
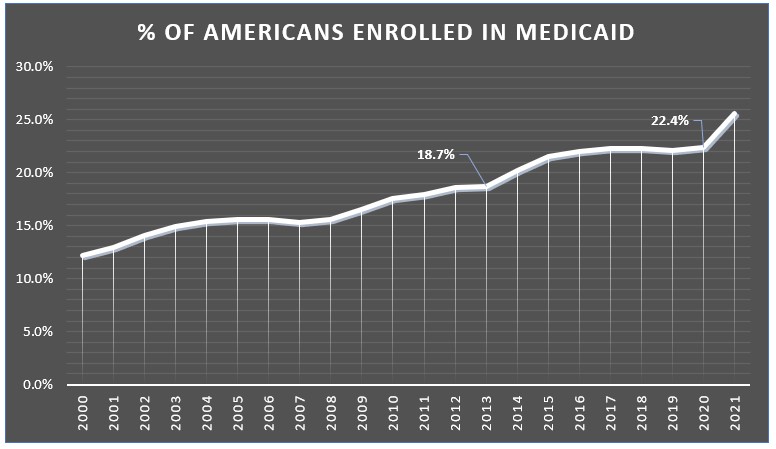
Multiplying that by costs per enrollee and the total population, the cost in 2020 for expanding Medicaid was $112 billion. Applying that same approach to every year from 2014 to 2021, a combined $700 billion has been spent without achieving any mortality benefits.
From 2014 to 2021, a combined $700 billion has been spent without achieving any mortality benefits.
Even if we assume a 10% improvement in mortality, higher than either of the studies that found an effect, this works out to saving 560 lives per year and spending $200 million per life saved1, 20 times the value used by the EPA in their recently proposed social cost of carbon update.
Had a 10% improvement in mortality been achieved, Medicaid expansion would have spent $200 million per life saved, substantially more than policy-makers deemed effective.